Rehabilitation programs should always aim to be low-risk, high demand (Mendiguchia & Brughelli, 2011).
To create an effective therapeutic exercise program we need (Brody & Hall, 2011);
- sound clinical reasoning skills,
- an understanding of tissue healing,
- exercise prescription principles,
- motor learning principles, and
- knowledge of the intricate interplay between the cardiopulmonary, metabolic and nervous systems, biomechanical and psychological components are required
Also, we need to understand the environmental and personal factors that can aid decisions about appropriate interventions between patients that present with seemingly with similar musculoskeletal complaints. For example, a patient’s physical environment, workplace, or comorbidities, education and life experiences.
An exercise program can include targeting (Anemaet & Hammerich, 2014);
- muscular strength,
- power,
- endurance,
- aerobic exercise,
- balance,
- agility,
- coordination,
- gait retraining,
- ROM, or
- stretching
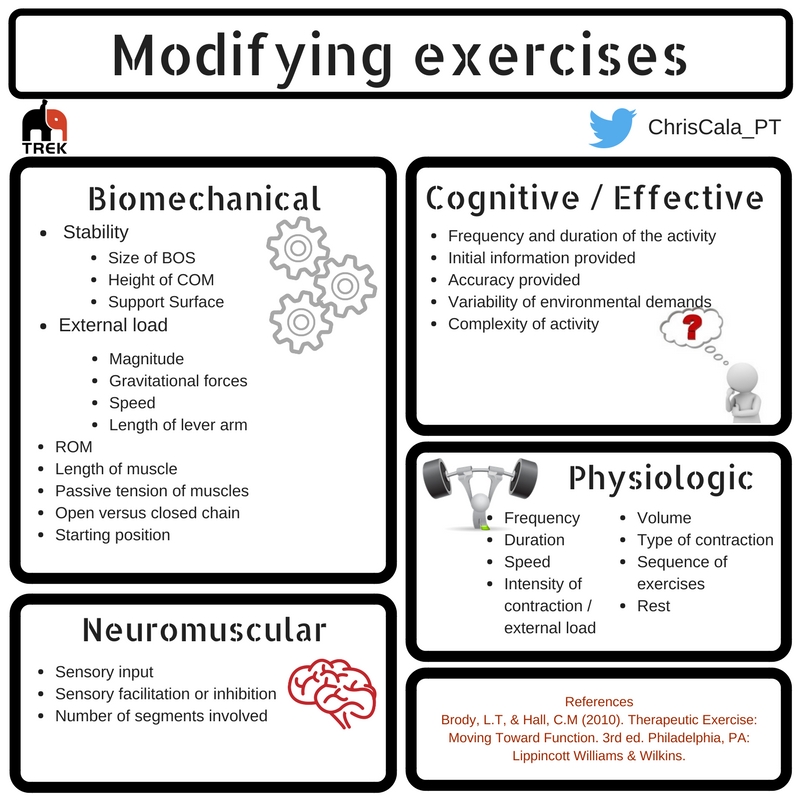
We do this through the manipulation of the intensity, duration, frequency, mode volume, and specificity of activity (Hoover, VanWye & Judge, 2016).
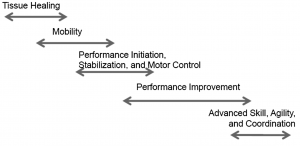
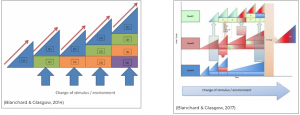
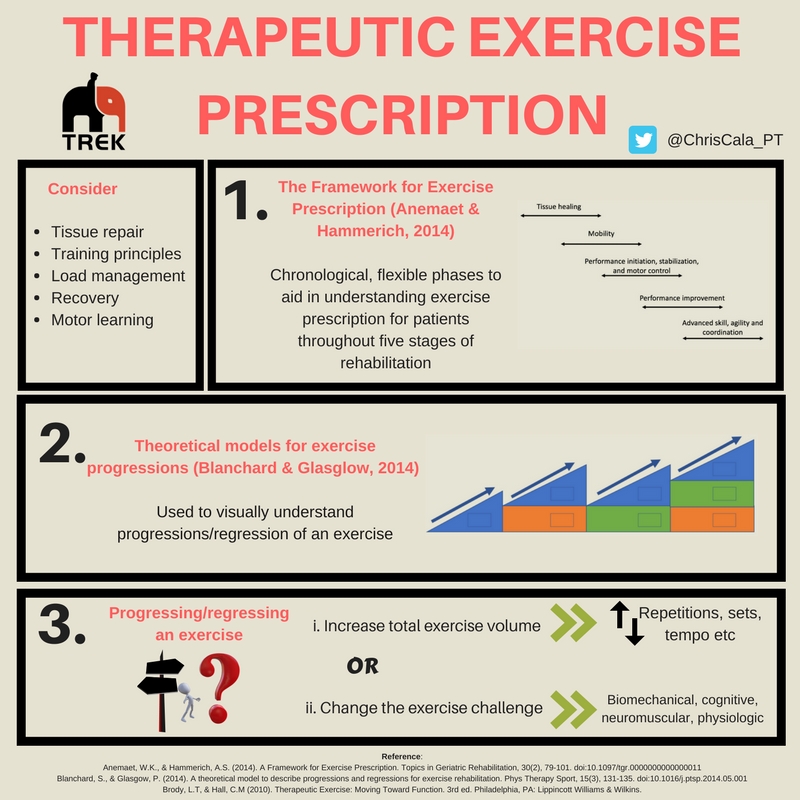
Below are 2 resources that can be used to assist with prescribing a therapeutic exercise program
- ‘Framework for Exercise Prescription’ (Anemaet & Hammerich, 2014) which is used to visualise phases of an exercise program, and
- ‘A theoretical model for exercise progressions’ (Blanchard & Glasgow, 2014 & 2017) which provides a visual representation of exercise progression and how they are incorporated into a larger program.
The Framework for Exercise Prescription (Anemaet & Hammerich, 2014)
This framework uses chronological, but flexible phases to aid in understanding exercise prescription for patients throughout five stages of rehabilitation including the (1) tissue healing phase; (2) mobility phase; (3) performance initiation/stabilisation and motor control phase, (4) performance improvement phase; and (5) advanced skill, agility and coordination phase
- ROM and isometrics are the most beneficial types of exercise in this phase.
- Controlled and progressive mobility is indicated to remodel tissues along the lines of tensile strength (Prentice, 2011).
- The timeframe at which tissue healing occurs depends on the type of tissue and the extent of the tissues damage.
Inflammatory phase: What does this mean for exercise prescription at this phase?
- Exercise aims to control inflammation through muscle contraction, in a pain-free range of motion to help minimise fibrosis (Anemaet & Hammerich, 2014).
- Early muscle injury rehabilitation improves return to sport timeframes (Bayer, Magnusson and Kjaer, 2017)
- However, if pain is reproduced in this stage, it may promote further tissue damage.
- Can be conducted in a PROM, AROM or A-AROM.
- Apply a gradual increase in stress on tissues to promote mechanotransduction and Wolff’s Law – tissues respond to the stressors placed upon them.
Proliferative phase: What does this mean for exercise prescription at this phase?
- Maximum strength hasn’t occurred during proliferation – the tissues integrity is restored with type 3 collagen before it is replaced by type 1 collagen in the repair and remodelling phases.
- Therefore, ROM and strengthening exercises must be continuously monitored for aggravation of symptoms or signs of inflammation.
Repair and remodelling phase: What does this mean for exercise prescription at this phase?
- As the remodelling phase begins, more aggressive active range of motion and strengthening exercises should be incorporated to facilitate tissue remodelling and realignment along the lines of stress.
- Range of motion and muscle contraction exercises are valuable interventions, although the risk of further injury still exists and can ultimately delay tissue healing.
- Intensity should be low, and the duration kept short, with continual monitoring of patient symptoms. Progressively increasing intensity is still very important.
Some patients can skip straight to this phase if signs and symptoms of inflammation and if initial proliferation stages have occurred.
- If signs of inflammation have disappeared, are showing signs of decreasing, or are not worsened with the mobility activity for greater than 24hours, patients can progress to this phase.
- Exercises in this phase can include ROM exercises, stretching exercises, or even eccentric exercises for lower limb mobility (O’Sullivan, McAuliffe & Deburca, 2012).
- Determining which ROM exercise to use is dependent on patient irritability and what type of mobility impairment is present (Brody, 2012). For example, a patient may present with restricted range due to joint restrictions, pain, muscle or oedema, hypermobility or joint instability. If there is a mobility restriction, it should be determined if it is due to an arthrokinematics limitation (how the joint moves – generally treated with a joint mobilisation intervention), or a osteokinematic limitation (how the bones move – generally treated using ROM exercises).
- Forcing joints through bony restrictions, recent trauma, acute inflammation or infection is contraindicated. Furthermore, mobility exercises are not required in all patients, e.g. patients with a spinal cord injury may not benefit from stretching of the hamstrings as they might utilise them for stability in sitting.
Some patients can skip directly to this stage if signs of inflammation are absent, decreasing, or are not worsened with the introduction of these exercises for greater than 24hours. Patients should however be in proliferative or remodelling stages of healing.
- Full mobility is also not required to begin this stage, but a pain-free range to exercise is essential.
- Exercises in this phase are completed daily, with a high number of repetitions and a low weight (<50%1RM for isotonic exercises OR 25-50%MVC for isometrics) which allows the body to maintain a predominately aerobic supply of energy.
Improving muscle initiation;
- Successful muscle initiation requires neural, vascular, metabolic and muscular contribution and is concerned with the physiological sequence of events of a muscle contraction.
- Muscle contraction and initiation are essential to enable full tissue healing as they induce tissue adaptation, introduce stress and aid in joint stability and motor control for functional activities.
- Concentric, eccentric and isometric exercises can also be used in this phase. To distinguish their use between phases, the dosage parameters are manipulated.
- To decide the most appropriate muscle action, apply the principle of specificity – i.e. does the muscle need to act eccentrically/concentrically/isometrically? Does it need to work in an open-chain versus closed chain environment?
- This phase requires specific and accurate prescription dependent on the functional tasks that are required – this will include what biomotor abilities are most involved in this functional task. For example, strength, hypertrophy, power or endurance and muscle contraction type.
- While there is the crossover effect within biomotor abilities, it is important to apply the principle of specificity to the patient’s functional limitations to determine the training goal, as this will result in the best outcomes (Mangione, Miller & Naughton, 2010).
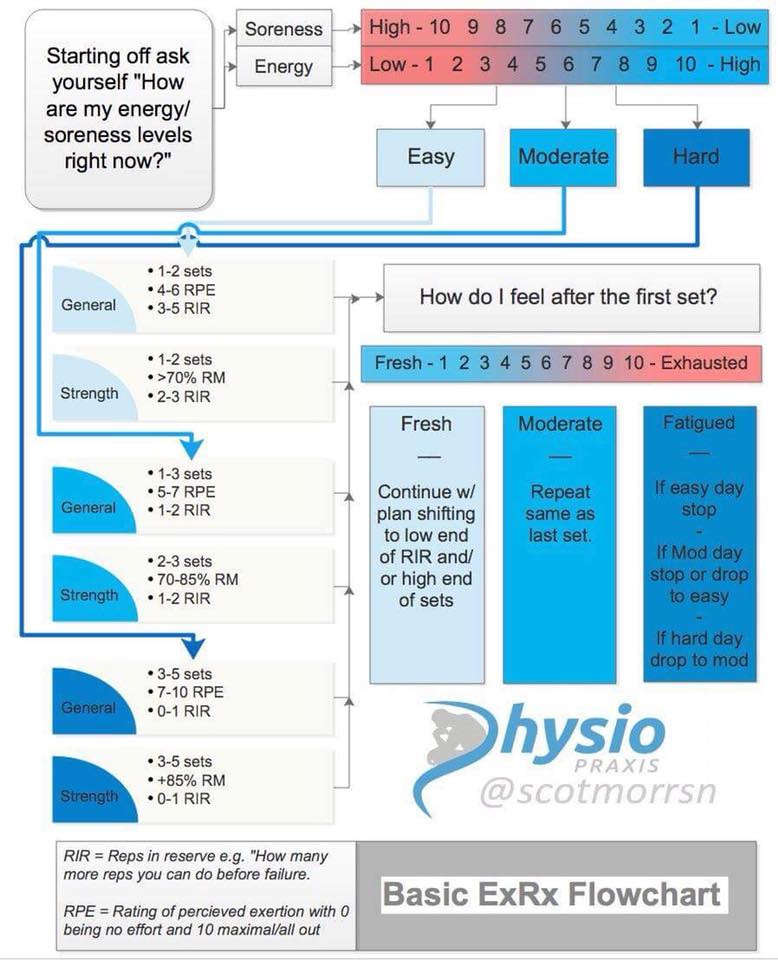
- Consideration of contextual factors that can impact on exercise prescription should be considered which allows the clinician to improve their exercise dosages to compliment these factors by adjusting for daily activity loads (Brody, 2012).
- What environmental (i.e. work demands) and personal factors (i.e. unsupportive family, work ethic) are present? Do these positively impact or negatively impact rehabilitation?
- Once the training goals component has been identified, the muscle action (concentric, eccentric or isometric), load, reps & sets, positioning, order, rest periods, velocity and frequency parameters are decided.
Once patients have progressed through rehabilitation and have approached near-normal muscle performance without signs of tissue injury or mobility limitations, they begin to integrate components from previous phases to higher-level coordination and skill movements by adding plyometrics or manipulating body position, surfaces, resistance, agility or coordination.
NOTE: This stage is not solely for those returning to competition or sport.
For example, adding perturbations during single leg landing drills for those with balance deficits
- Plyometric exercises produce power through combining strength and speed which utilise the physiological properties of stretch reflexes and the musculotendinous-junction (MTJ) to increase motor unit recruitment and ultimately force production (Turner & Jeffreys, 2010).
- They can act as injury prevention, can improve joint ROM and flexibility and especially important for movements requiring a quick transition from concentric to eccentric muscle action.
Theoretical models for exercise progressions (Blanchard & Glasglow, 2014; Blanchard & Glasglow, 2017)
These rehabilitation models can be used for visually understanding progressions/regression of exercises. They can be used as adjuncts to the Framework of Exercise Prescription.
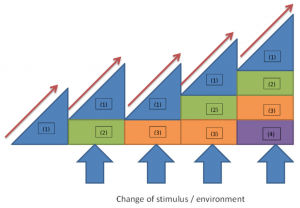
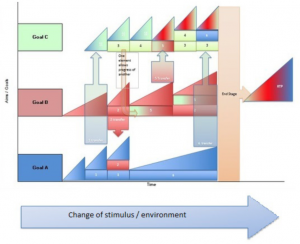
- Consider the stage of healing, relevant impairments and appropriate contextual factors to create goals
- List the goals of rehabilitation that will lead to achieving functional goals along the vertical axis. These goals will be both achievable and challenging and can be an individual skill, or a set of skills e.g. improve ROM or hopping or return to running.
- The horizontal axis represents time and the vertical axis the level of difficulty of the exercise.
- Choose a starting exercise. The first triangle (1) of Blanchard & Glasgow’s model is the safest and most controlled level of the exercise. The (1) doesn’t fundamentally change throughout the rehabilitation. The exercise in this first triangle will stay as an exercise where implicit processes are dominant (i.e. an external stimulus is not added yet).
- Advancing through the rehabilitation requires progressing exercises. This is represented within the model along the horizontal axis through the red arrows (represents manipulating frequency, intensity or duration) OR the boxes added to the initial triangle and denoted by ‘(2), (3), (4)’ etc… (changing the stimulus or environment)
An important skill in rehabilitation is to be able to identify appropriate impairments that are contributing to the activity limitations which aids in prioritisation of exercises. If an impairment has been linked to activity limitations, consider (Brody & Hall, 2011);
1. Is the impairment amenable by physiotherapy?,
2. What are the potential negative effects of the exercise for that impairment?
3. What is the cost:benefit ratio of the exercise for that impairment? and,
4. Can it lead to future impairment if left untreated?
Considerations to acknowledge when creating an initial program include with the goal to challenge the individual to expand the training volume to bridge the gap between current, and desired function (Brody & Hall, 2010):
– Which muscle groups require training, which other muscles work with it, and which contraction type is needed for functional activities
– What range or position does the muscle have to function? At what speed?
– What type of training is required? i.e. strength, endurance, power or hypertrophy
– What is the patient’s training history/current status?
– What is the most appropriate way to load tissues for this patient given their history/current status?
– What precautions are present?
– What stage of healing is most likely?
Ultimately, there are two overarching ways to progress the initial exercise to continuously challenge the patient but must remain in balance with exercise load and daily load (optimal loading).
1. Increase the total exercise volume
– Can be applied by increasing frequency, intensity or duration when the current volume is tolerated by the patient without an increase in symptoms
– The amount of volume increased depends on the current function versus the functional goal (Brody & Hall, 2012)
– An increase in volume is represented by the red arrows throughout the above models
2. Change the exercise challenge without directly increasing total exercise volume
Can be applied when:
– an increase in volume may not be indicated because of tissue healing stages, OR
– if an increase in volume exacerbates the patients symptoms, OR
– if patient contextual factors inhibit the ability to increase volume i.e. physical job
Types of challenge variables
- NB: While volume is not directly manipulated, the type of stress on tissues is changed and challenges the motor control of the initial exercise. Therefore, there should be a concurrent regression in the duration, speed, distance and other parameters previously prescribed to protect healing tissue and to minimise potential overloading.
- NB: It is common in patients who are at later stages of rehabilitation and those who demonstrate stable symptoms, to progress exercises using a flexible approach with an increase in volume being balanced concomitantly with a challenge variable. Conversely, if the patient demonstrates unstable symptoms, exercise changes should be kept to a minimum to ensure changes to symptoms can be identified and modified.