In a section aiming to discuss the science of pain, it is fair to start with two assumptions:
1) Pain is complex.
2) Pain requires an explanation.
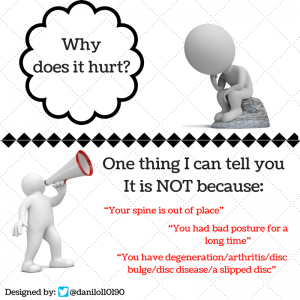
The complexity of pain often leads health professional to provide wrong or misleading explanations to patients. It can be quite important to understand what factors are more likely to make the pain worse (e.g. anxiety, depression, insomnia) and factors that are often reported as “cause” of pain, but, actually are not even related with pain (e.g. bad posture, spine out of place, crepitus).
In this section you will have the opportunity to enhance your knowledge about aspects of the science of pain.
Start watching a brilliant talk by Lorimer Moseley
Pain can be classified into two broad categories: Nociceptive pain and Neuropathic pain.
These categories can be metaphorically explained by a broken mobile phone. In the first case the mobile phone slipped from your hand and was crashed on the floor (nociceptive pain); In the second case, your mobile phone is physically fine but the microprocessor responsible for making everything work well has having some trouble, so, many functions of your mobile phone are not working well (neuropathic pain).
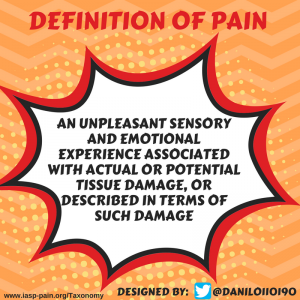
Below you will find the IASP definitions for nociceptive and neuropathic pain:
Nociceptive pain
Pain that arises from actual or threatened damage to non-neural tissue and is due to the activation of nociceptors.
Note: This term is designed to contrast with neuropathic pain. The term is used to describe pain occurring with a normally functioning somatosensory nervous system to contrast with the abnormal function seen in neuropathic pain.
Neuropathic pain
Pain caused by a lesion or disease of the somatosensory nervous system.
Note: Neuropathic pain is a clinical description (and not a diagnosis) which requires a demonstrable lesion or a disease that satisfies established neurological diagnostic criteria. The term lesion is commonly used when diagnostic investigations (e.g. imaging, neurophysiology, biopsies, lab tests) reveal an abnormality or when there was obvious trauma. The term disease is commonly used when the underlying cause of the lesion is known (e.g. stroke, vasculitis, diabetes mellitus, genetic abnormality). Somatosensory refers to information about the body per se including visceral organs, rather than information about the external world (e.g., vision, hearing, or olfaction). The presence of symptoms or signs (e.g., touch-evoked pain) alone does not justify the use of the term neuropathic. Some disease entities, such as trigeminal neuralgia, are currently defined by their clinical presentation rather than by objective diagnostic testing. Other diagnoses such as postherpetic neuralgia are normally based upon the history. It is common when investigating neuropathic pain that diagnostic testing may yield inconclusive or even inconsistent data. In such instances, clinical judgment is required to reduce the totality of findings in a patient into one putative diagnosis or concise group of diagnoses.
Some medical conditions don’t fit into the two categories cited above (e.g. fibromyalgia, complex regional pain syndrome). Some terms have been proposed in order to fit such medication conditions in categories:
Nociplastic pain
Pain that arises from altered nociception despite no clear evidence of actual or threatened tissue damage causing the activation of peripheral nociceptors or evidence for disease or lesion of the somatosensory system causing the pain.
Note: Patients can have a combination of nociceptive and nociplastic/algopathic/nocipathic pain
This short video will help you to understand pain in a clear way.
Physical activity and exercise can help pain management. A recent overview of Cochrane reviews reported that physical activity reduced the severity of pain, improved physical function, and had a variable effect on both psychological function and quality of life.

Can exercise lead to adverse events?
According to the available evidence, physical activity did not cause harm. Muscle soreness that sometimes occurs with starting a new exercise subsided as the participants adapted to the new activities. This is important as it shows physical activity in general is acceptable and unlikely to cause harm in people with chronic pain, many of whom may have previously feared it would increase their pain further.