Exercise and aging
Older adult defined as ≥ 64 years+
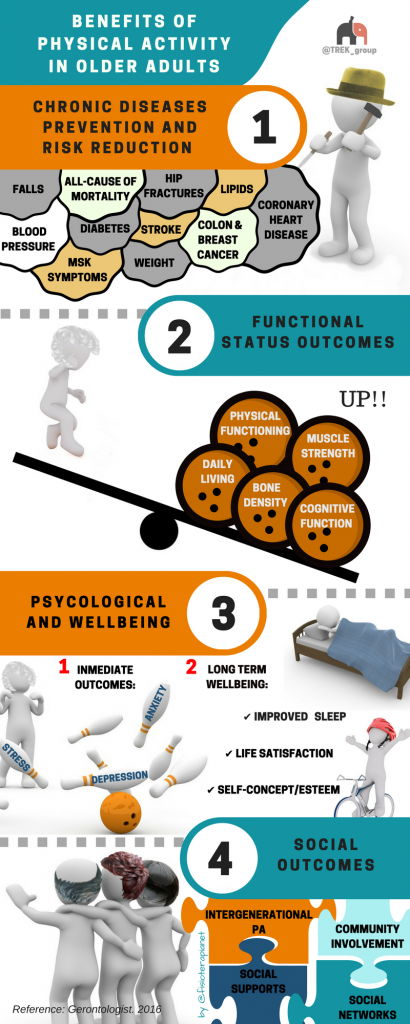
- Muscle strength decreases by more than 10% each decade (Lynch, Metter et al. 1999)
- Weakness is associated with decreased bone mineral density (Bevier, Wiswell et al. 1989)
- Strength training is important to reverse these age-related changes
- Prevention over cure
- Recommended levels of physical activity for ≥ 64 years+
- See Blood flow restriction for improvement in physical function and walking in older adults.
Assessment:
- ESSA Adult Pre Exercise Screening Tool
- Aerobic Endurance Test (with normative values for female and male)
Strength after Sixty:
“Doing squats won’t kill you even if you’re old”
Recommendations:
- Use functional strength training that incorporates balance and co-ordination
- Progressive overload – The muscles of older adults need to be challenged in order to grow just as the muscles of younger adult
- Neuromuscular training – take advantage coordination and complex movements to challenge the brain
- Movement standards refer to Exercise technique guidelines
Best Exercises:
- Double leg Bridge: neuromuscular training of the pelvic gluteal activation sequence as well as spinal articulation and control.

- Single Leg Bridge: Strength progression as well as isolation, balance and coordination.

- Squats: The Squat is very important movement to get right as it mimics sitting down, jumping and many everyday life movements you need in order to live!
- When you improve squat strength, you are developing strength in a sequence that the brain can immediately apply to similar movements, such as walking up stairs, because it shares a similar relative timing sequence.

- Deadlift: how often you would need to bend over in a day? We use this movement all the time and don’t think about it.
- Performing this exercise in a control environment can improve your everyday ability to pick something off the floor

Resistance program:
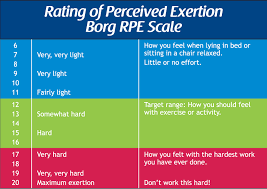
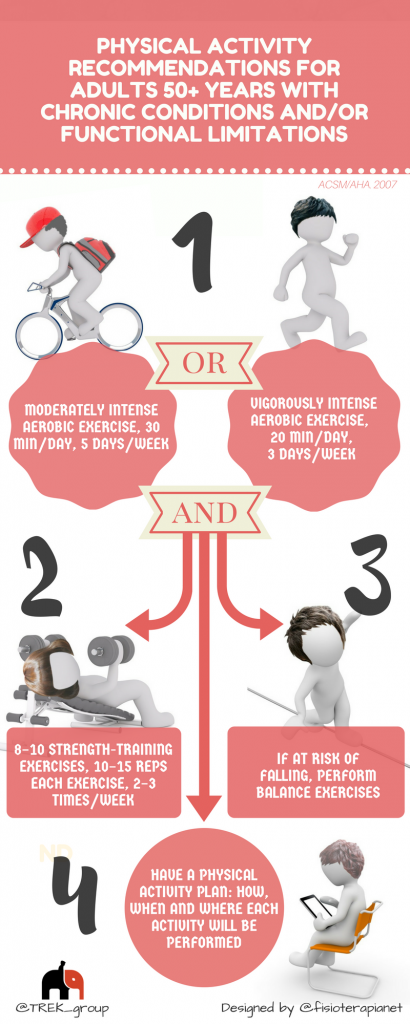
- Training program recommendations:
- 8-10 exercises
- 2 -3 sets of 6-12 repetitions of each exercise
- 70-80% of the one repetition maximum (1-RM)
- 2-3 times per week
- Program length: for periods ranging from six weeks to two years.
- Dosage and progression as per novices
- Slow progression for those with:
- Hypertension
- Arthritis
- cardiovasular disease
- other conditions that limit function
- Setting and supervision: initial instruction and performance in a supervised setting are important
Supporting articles/text
- Marlow, N., Hastings, K., & Hansson, J. (2014). Exercise & Sports Science Australia’s Outcome Measures for Exercise physiologists: Ensuring Evidence Based Practice. Exercise & Sports Science Australia.
- Mackenzie, B. (2005). 101 Performance Evaluation Tests. London. Jonathan Pye.
Falls prevention
Prevalence:
Falls affect a significant number of older Australians, with over one-third of community dwelling people aged 65 years and older falling one or more times every year.
Falls can also result in disability, loss of mobility, reduced quality of life and fear of falling.
Definition:
Falls defined as “unexpected events in which the partic- ipant comes to rest on the ground, floor, or lower level”.
Risk factors:
- reduced muscle strength
- impaired balance and gait
Exercise Prevention:
ACSM guidelines state that To reduce risk of injury from falls, community-dwelling older adults with substantial risk of falls (e.g. with frequent falls or mobility problems) should perform exercises that maintain or improve balance
Recommendations:
- ACSM/AHA physical activity guidelines for all adults aged 65+ years and adults age 50–64 years with clinically significant chronic conditions and/or functional limitations
Balance Testing:
Balance exercises:
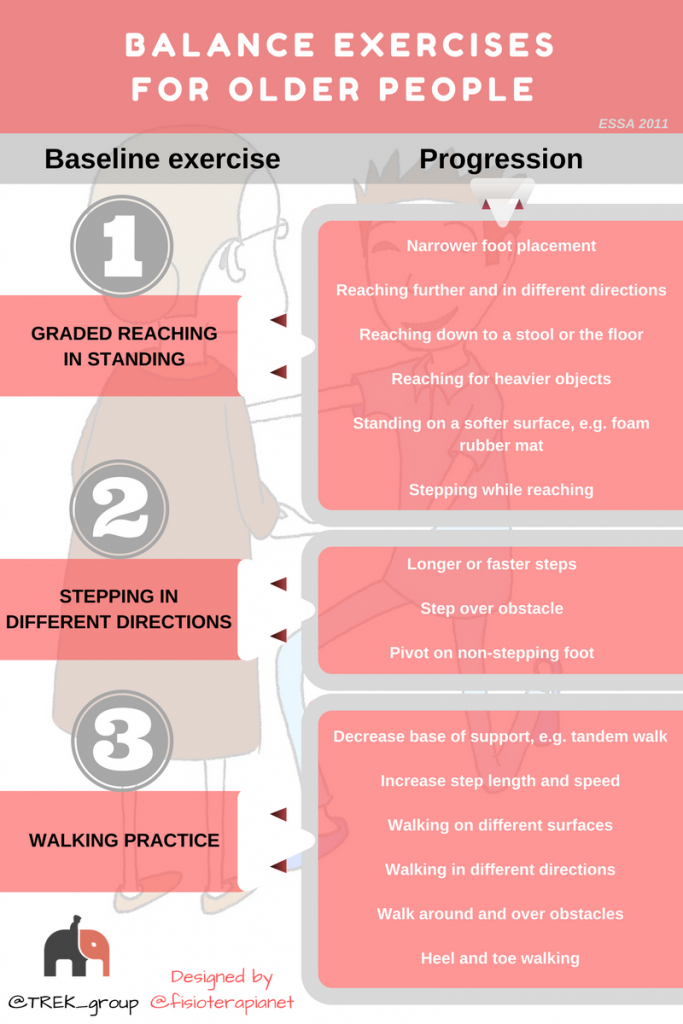
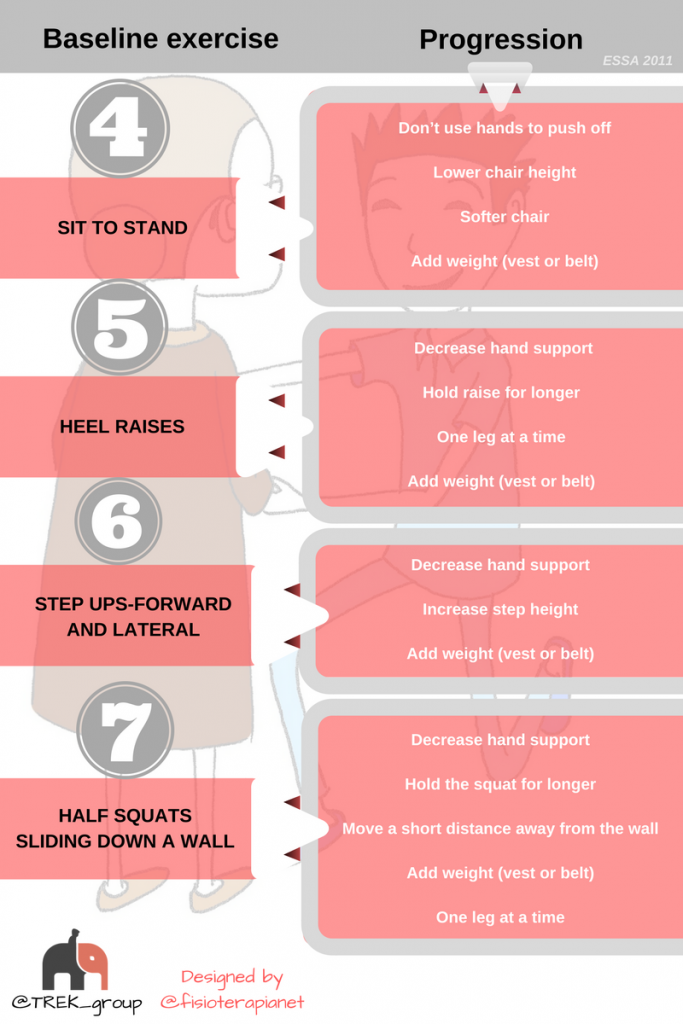
Otago Exercise programme including:
- Assessment
- Resistance program
- Balance program
- ESSA position statement Falls prevention: